A Healthy endometrium is necessary for a successful pregnancy. However, many women struggle with a condition known as Thin Endometrial, which can interfere with conception and lead to complications in fertility treatments like IVF. Understanding this condition, its symptoms and causes is key to early diagnosis and effective management.
In this blog, we’ll explore what Thin Endometrial means, how it affects your fertility and why timely consultation with an IVF Specialist in Mumbai can make a significant difference.
What is Thin Endometrial?
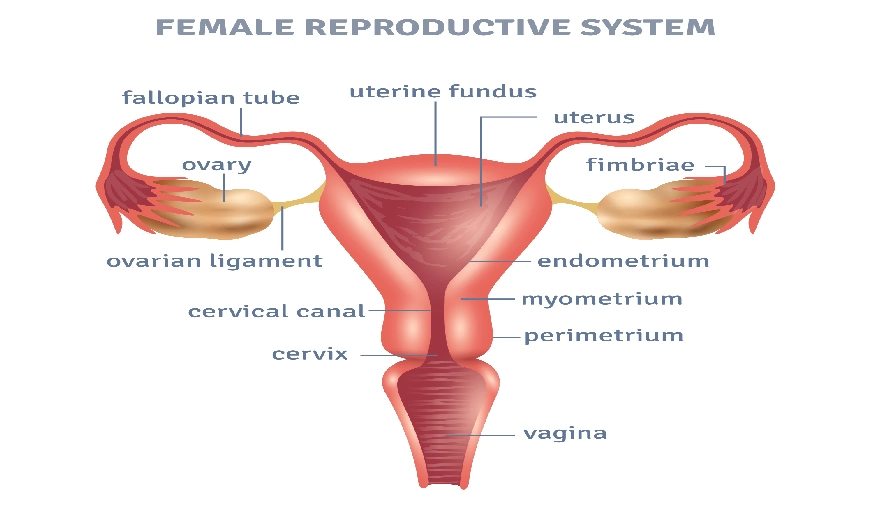
The endometrium is the inner lining of the uterus, which thickens every month in preparation for pregnancy. If fertilization doesn’t occur, this lining is shed during menstruation.
A Thin Endometrial lining is typically defined as being less than 7 mm in thickness during the implantation window of a woman’s menstrual cycle. Ideally, for embryo implantation to occur, the lining should be at least 8-12 mm thick. A thinner lining can prevent the embryo from implanting properly or result in early miscarriage.
Common Symptoms of Thin Endometrial
Many women with a Thin Endometrial lining may not experience obvious symptoms, especially in the early stages. However, some potential signs include:
- Irregular menstrual cycles
- Light or scanty periods
- Difficulty conceiving naturally
- Early pregnancy loss or failed IVF cycles
Causes of Thin Endometrial
There are several reasons why a woman may develop a Thin Endometrial lining. Identifying the root cause is recuire for effective diagnosis and fertility planning.
1. Hormonal Imbalances
The hormone estrogen primarily regulates the growth of the endometrial lining. When estrogen levels are low due to conditions like Polycystic Ovary Syndrome (PCOS), menopause or issues with the pituitary gland the lining may not thicken as required. An imbalance between estrogen and progesterone can further disrupt the endometrial cycle, affecting fertility and increasing the risk of implantation failure during IVF treatments.
2. Uterine Infections
Chronic infections, especially endometritis or genital tuberculosis (a more common issue in certain regions), can damage the endometrial tissue over time. These infections may go unnoticed for years, silently causing inflammation and scarring. As a result, the uterus becomes less receptive, and the lining may remain thin, leading to repeated implantation failures or miscarriages.
3. Previous Uterine Surgery or D&C Procedures
Surgical interventions like dilation and curettage (D&C), hysteroscopic polyp removal, or cesarean sections can injure the endometrial tissue. When this damage results in scar tissue formation inside the uterine cavity, it may lead to Asherman’s Syndrome. In such cases, the scarred endometrial lining loses its ability to regenerate and respond to hormonal signals, remaining thin throughout the cycle.
4. Poor Blood Flow to the Uterus
Adequate blood circulation is essential for delivering oxygen and nutrients to the endometrial tissue. When blood flow to the uterus is compromised due to a sedentary lifestyle, smoking, uterine fibroids, or even certain structural abnormalities, the endometrial lining may not develop fully. A thin and poorly perfused endometrium lacks the richness and vascularity needed for embryo implantation.
5. Prolonged Use of Fertility Medications
While fertility medications aim to stimulate ovulation and improve conception chances, excessive or prolonged use without proper monitoring can have adverse effects. Overstimulation from repeated IVF cycles or use of clomiphene citrate, for example, may desensitize the endometrial lining to estrogen, making it thin and unresponsive. In such cases, even high-quality embryos may fail to implant.
How Thin Endometrium Affects Fertility
For couples trying to conceive, a Thin Endometrial lining can significantly reduce the chances of a successful pregnancy. Since the embryo requires a thick, nutrient-rich environment to implant and grow, any deficiency in the endometrial layer can lead to implantation failure.
This is especially important for women undergoing assisted reproductive techniques. Consulting the Best IVF doctor in Mumbai can help evaluate the quality of the endometrium and recommend personalized treatment options.
Diagnosis and Evaluation
The most common method to measure endometrial thickness is transvaginal ultrasound, typically performed around day 12-14 of the menstrual cycle. In some cases, additional tests like hysteroscopy, endometrial biopsy, or color Doppler studies may be recommended to assess blood flow and detect underlying abnormalities.
When to See a Fertility Specialist
If you’ve been trying to conceive for over 6-12 months without success, or if you’ve had failed IVF attempts, it’s time to consult the Best IVF Doctor in Mumbai. A fertility expert will guide you through a series of tests and tailor a treatment plan based on your unique medical history and uterine health.
Mumbai is home to some of the most renowned fertility clinics and specialists. The Best IVF doctor in Mumbai will not only focus on ovulation and egg quality but will also ensure your uterus can support a healthy pregnancy.
To Conclude
A Thin Endometrial lining might seem like a small issue, but it can significantly affect your fertility journey. With the right diagnosis and a personalized treatment approach, many women have successfully overcome this challenge and achieved a healthy pregnancy. If you’re facing difficulties with conception, don’t wait. Seek help from an IVF Specialist in Mumbai to ensure every part of your reproductive system, including your endometrial health, is optimized for success.