
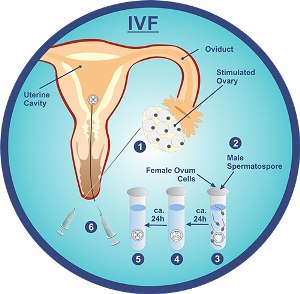
IVF stands for in vitro fertilization. It refers to the process by which a woman’s eggs are collected and then fertilized outside her womb in the test tube baby centre in Mumbai laboratories .
This is done in a Petri dish (“in vitro” is Latin for “in glass”) where the collected eggs are kept and the washed semen containing sperms is added to it so that one of the sperms fertilizes the egg.
The fertilized eggs (embryos) are cultivated and grown in the laboratory and after appropriate growth; they are transferred back to the uterine cavity.
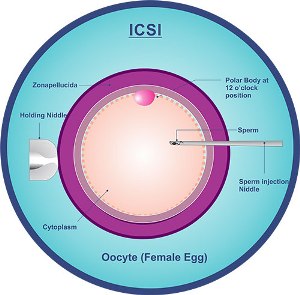
ICSI is a form of gamete (sperm and egg) micromanipulation that involves the direct injection of a single sperm into the cytoplasm (inside portion) of an oocyte (egg).
ICSI is an acronym for “Intra Cytoplasmic Sperm Injection” – which is a long, fancy way of saying “inject sperm into the middle of the egg”.
ICSI is a very effective method to get fertilization of eggs in the test tube baby centre in Mumbai lab after they have been retrieved from the female partner.
IVF with ICSI involves the use of specialized micro-manipulation tools and equipment and inverted microscopes that enable embryologists to select and then pick up individual sperms in a tiny specially designed hollow ICSI needle. The sperms are first inactivated by breaking their tails. (Hence ICSI is mostly used in males with severe motility disorder, severe asthenozoospermia)
Then the needle is carefully advanced through the outer shell of the egg and egg membrane and the sperm is then injected into the inner part (cytoplasm) of the egg. This will usually result in normal fertilization in approximately 70-85% of eggs injected with viable sperm.
Couples who require test tube baby treatment include:
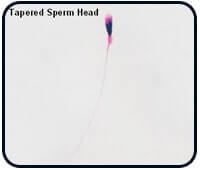
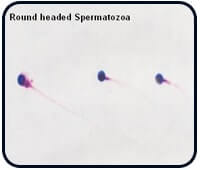
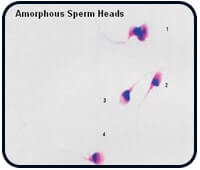
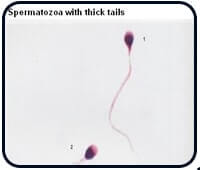
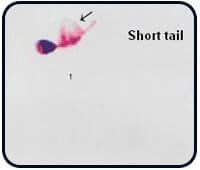
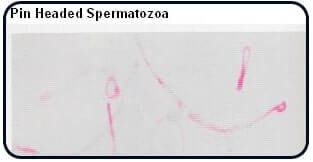
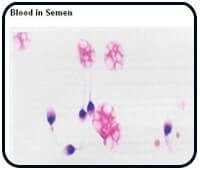
Pictures showing different kinds of sperm morphologies Click Below link.
Normal Sperm,Tapered sperm head, Round-headed sperm, Amorphous sperm head, Elongated sperm head & sperm with double head.

ICSI Treatment has proved to be very useful in couples who had Failed IVF Treatment earlier in achieving fertilization or had very poor fertilization where the male partner has abnormal sperm parameters like severe oligospermia (very low count), severe asthenozoospermia (very less motility), severe teratozoospermia (high percentage of abnormal sperms) or a combination of abnormalities like oligoasthenoteratozoospermia (very low count, poor motility, abnormal sperms).
ICSI also can be performed in azoospermic men (where semen sample contains no sperms).
In such cases the testis are producing sperms but due to block in the tubules or in the path through which the sperms come out from the testis, the sperms produced in the testis cannot come out.
ICSI has proved to be very useful in couples who have failed to achieve fertilization or had very poor fertilization following standard IVF treatment & in couples where the male partner has abnormal sperm parameters like severe oligospermia (very low count), severe asthenozoospermia (very less motility), severe teratozoospermia (high percentage of abnormal sperms) or a combination of abnormalities like oligoasthenoteratozoospermia (very low count, poor motility, abnormal sperms).
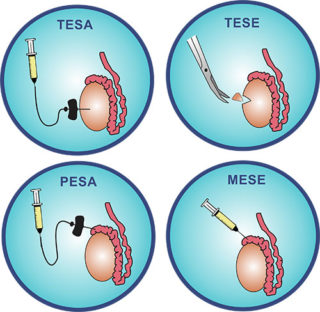
ICSI also can be performed in azoospermic men (where semen sample contains no sperms). In such cases the testis are producing sperms but due to block in the tubules or in the path through which the sperms come out from the testis, the sperms produced in the testis cannot come out. Here the sperms are obtained microsurgically from testis or epididymis (PESA, TESA, and TESE)*. In a few cases when there is a severe abnormality in the semen, testicular extraction by microsurgical approach (PESA, TESA & TESE) has given normal sperms.
*PESA- Percutaneous Epididymal Sperm Aspiration
TESA – Trans Epididymal Sperm Aspiration
TESE – Testicular Sperm Extraction
TESA or testicular sperm aspiration (also known as TESE, or testicular sperm extraction) is one of the surgical sperm harvesting techniques used for retrieving sperm in patients with azoospermia. A number of surgical sperm retrieval or recovery methods have been devised to recover sperm from the male reproductive tract.
In men with obstructive azoospermia,(because of duct blockage or absence of the vas deferens), sperm are usually recovered from the epididymis. The original technique was devised by a urologist, Dr. Sherman Silber, who is a specialist in microsurgery. It is a very simple and easy method to recover sperm from the blocked epididymis. Since the surgeon can feel the turgid epididymis, swollen with sperm, he will blindly puncture the epididymis using a simple butterfly needle – a technique that was very similar to drawing blood from a blood vessel! This simple technique is called PESA (percutaneous epididymal sperm aspiration), in which the sperm is sucked out from the epididymis by puncturing it with a fine needle.
For patients with obstructive azoospermia in whom sperm cannot be found in the epididymis, it is always possible to find sperm in the testis. The easiest way to retrieve this is through TESA or testicular sperm aspiration, in which the testicular tissue is sucked out through a fine needle, under local anesthesia. The testicular tissue is placed in culture media and sent to the lab, where it is processed. The sperm are liberated from within the seminiferous tubules (where they are produced) and is then dissected free from the surrounding testicular tissue.
The purpose of IVF treatment is to bypass the fallopian tube where fertilization normally occurs, so that we can overcome tubal factors if it is one of the factors causing infertility.
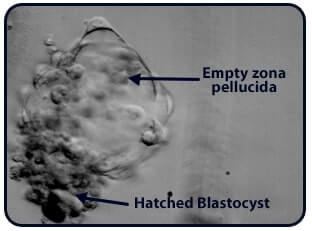
IVF / ICSI can also bypass mechanical factors, sperm defects like acrosome defect, or oocyte defects like zona pellucida being too thick. With IVF treatment/ICSI, subtle hormonal defects get corrected and endometrial receptivity improves. Unexplained infertility may be due to one of the above factors and may get corrected by IVF treatment/ICSI treatment cycle at Ankoor test tube baby centre in Mumbai.
In the month prior to the IVF Treatment stimulation cycle, medications/injections are given to suppress the body’s natural hormones so that the subsequent stimulation of ovaries is better controlled.
You may be put on birth control pills in this cycle. This may seem strange – you are trying to get pregnant and we are putting you on birth control pills. Actually, though, using birth control pills before a treatment cycle has been shown to decrease your risk of ovarian hyperstimulation syndrome (OHSS) and ovarian cysts and hence may improve the chances of success. It also causes suppression of LH hormone and suppression of the entire cohort of follicles so that all the follicles are in the same phase and will grow simultaneously.
Option 1:
Another possible option is that we monitor your follicular growth and ovulation and give you estradiol valerate tablets until you get your periods. This is to suppress the FSH hormone in your body which helps in follicle recruitment. If the body’s FSH is suppressed, we can recruit more number of follicles by giving injections. Suppression of FSH does not allow the natural selection of the follicle by the body, thereby uniform recruitment of the follicles and we will get more number of follicles.
Option 2:
Sometimes we monitor your follicular growth and ovulation and start Injection Lupride. This is used in the long protocol of IVF treatment and the basic aim is the same – to suppress the body’s natural hormones so that all the follicles (cohort) are maintained at the same size and can grow equally.
The type of protocol differs from patient to patient, depending on their age, previous response, endometrial lining etc.
Generally, the husband is told to give one semen sample before the start of the cycle. This sample will be frozen until the day of actual oocyte retrieval. This is because the stress of the day and anxiety can make it difficult for some to give the semen sample on the day of oocyte retrieval. So just in case that happens, at our test tube baby centre in Mumbai we will have a backup sample.
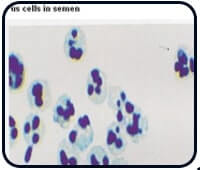
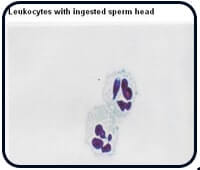
Oocyte retrieval, as well as embryo transfer, takes place through the vaginal route. Therefore if there is any vaginal infection, it may be transmitted to the ovaries or the uterus. This may hamper the results of IVF treatment. Even infection in the male genital tract can affect the results and more importantly, can be a source of transmission to the female partner. Treating genital tract infection is very important. Therefore, at our test tube baby centre in Mumbai we give a course of oral antibiotics to both the husband and wife in order to clear the genital tract of any infection. In addition, vaginal peccaries (a combination of antibiotic and antifungal preparation) are given to clear the vaginal tract of any infection.
This is when we at our test tube baby centre in Mumbai actually start the expert IVF treatments/ICSI cycle. You will need to come on day1/day2 of periods. A baseline ultrasound is performed to rule out ovarian cysts. If a cyst is present, the cycle may be postponed to next month or the cyst can be aspirated and the cycle can be started.
If required, baseline hormone levels like Serum E2 and LH are tested. This is to make sure your ovaries are “sleeping” or are suppressed so that the stimulation of ovaries with (Gonadotrophins) HMG /FSH injections will happen correctly.
PRINCIPLE – In a natural cycle, a woman’s ovaries will generally produce one egg. But when we are doing an invasive procedure like expert IVF treatments/ICSI it is better to have more eggs which will maximize the chances of success. Also, not all stimulated follicles are mature and give eggs. In addition, there is a limited rate of fertilization (all the eggs that are obtained do not fertilize). What would we do if a single egg we obtain does not fertilize? If we have more eggs, we can make more embryos and select the best embryos for transfer.
Hence injections are given to obtain controlled ovarian stimulation (COS).
At our test tube baby centre, ovarian stimulation is achieved by daily injections of gonadotropins, which are given subcutaneously and can be self-administered. At our test tube baby centre in Mumbai, we teach you how to take injections and 99% of patients take them on their own without any problems. This helps you to cut down on hospital visits or running to your family doctor daily just to take the injections which waste lots of time and creates unnecessary anxiety.
The stimulation process is monitored by serial ultrasounds and blood tests, which are done as and when required. The first ultrasound is generally done on the 4th /5th day of stimulation. This helps us to monitor the growth of your follicles and assess whether the dose of the injections needs to be increased, decreased or remain the same. The next ultrasound is 2 days later and then it is generally on alternate days or daily till the follicles are ready (approximately 18 to 20mm in size on USG). Transvaginal ultrasound not only helps to monitor the follicular growth but also helps to monitor the endometrial thickness.
These injections generally continue till the follicles are ready which is usually for 8 or 9 days. This comes to around 9th -11th day of periods.
When the follicles in the ovaries are ready (18-20mm) HCG injection is given for oocyte maturation. Timing this injection is vital. If it is given too early, the eggs will not have mature enough. If given too late, the eggs may be “too old” and won’t fertilize properly. The frequent ultrasounds are meant to time this trigger shot just right. At our test tube baby centre in Mumbai we usually give the HCG injection is when three or more follicles have grown to 17 to 19mm in size.
This is a minor surgical procedure that is performed on a daycare basis.
The egg retrieval takes place between 34 to 36 hours after you receive the HCG shot. It’s normal to be nervous about the procedure, but most women go through it without much trouble or pain.
You have to be fasting from midnight of the previous day of oocyte retrieval. On the day of oocyte retrieval, you have to come fasting (no tea, water etc). However, if you are taking any regular medications like that for thyroid, blood pressure, diabetes etc. you will take them in the morning with a sip of water (after confirming with us). When you come in, you will be taken in the ultrasound room for sonography and your husband will be sent to make admission papers. After the sonography, you will be taken to the recovery room where you will be given an OT changes (operation theatre gown). An IV line will be inserted and that is the only pain you will get! You and your husband will be given consent forms to sign. You will be taken to the operation theatre.
The oocyte retrieval is done under general anaesthesia with ultrasound guidance. Before the retrieval, an anesthesiologist will give you some medication intravenously to help you feel relaxed and pain-free. You are given general anaesthesia so that you will sleep completely for the entire procedure and will come to know nothing about the procedure. There is no intubation required. The whole procedure of oocyte retrieval usually takes about 15 to 20 minutes. The entire procedure is absolutely pain-free.
Once the medications take their effect, a transvaginal ultrasound is used to guide a needle through the back wall of your vagina, up to your ovaries. The needle is used to aspirate the follicle, and gently suck the fluid and oocyte from the follicle into the needle. One follicle generally contains one egg. But all the follicles do not contain an egg. On an average when we aspirate, we get one egg for every 2 follicles we aspirate. These oocytes once aspirated will be transferred to the embryology lab for confirmation of the number of eggs retrieved and further fertilization.
The number of oocytes retrieved varies but can usually be estimated before retrieval via ultrasound. The average number of oocytes is 5 to 10.
After the retrieval procedure, you’ll be taken to the recovery room where you will sleep off under the effect of anaesthesia for a couple of hours. Light spotting is common, as well as lower abdominal cramping, but most feel comfortable by the same evening. Once you get up you will be given a light snack. We will give you further instructions and you are ready to go home. Usually, the procedure is done in the morning and you are ready to go home by afternoon or evening.
The follicles that were aspirated will be searched for oocytes or eggs. Not every follicle will contain an oocyte.

Once the oocytes are found, they’ll be evaluated by the embryologist. If the eggs are overly mature, fertilization may not be successful. If they are not mature enough, the embryology lab may be able to stimulate them to maturity in the lab. This is called in vitro maturation which takes around 24 hours.


All the oocytes which are retrieved are carefully identified and kept in the CO2 incubator. During this period the semen sample is obtained from the husband and semen processing is done which isolates the healthiest sperms. The union of the male gamete (sperm) and female gamete(ovum) is known as fertilization. In test tube baby centre lab, fertilization is done either through IVF treatment or ICSI at Ankoor test tube baby centre in Mumbai
In an IVF, the embryologist places about 10,000 sperms in a culture dish with one oocyte.
With ICSI, which we generally prefer, the embryologist will choose a healthy-looking sperm and inseminate the oocyte with the sperm using a special thin needle.
The culture dishes are kept in a special incubator under special conditions (specified temperature and CO2 concentration) and after 24 hours, they are inspected for signs of fertilization.
The fertilization rate with ICSI is higher than IVF treatment. With ICSI, around 75 – 80% of the oocytes will get fertilized.
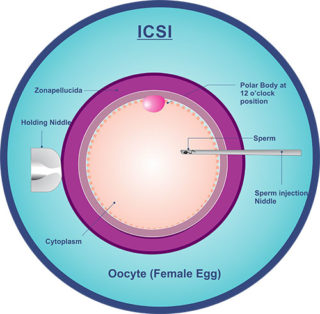
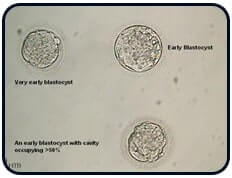
The above video shows the procedure of ICSI, wherein sperm is injected into the egg. This is followed by fertilization and formation of the embryo. It further shows the development of the embryo from one cell to 2 cells, 4 cell, morula stage and later developing into a Blastocyst (Day 5 Embryo)




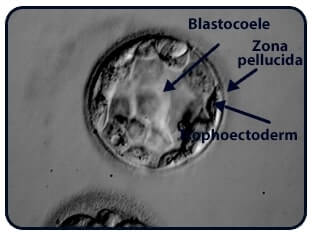
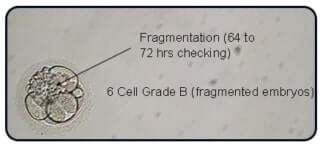
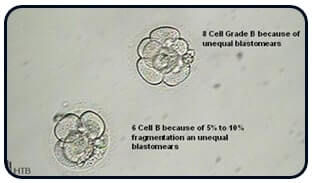
About three to five days after the retrieval, the fertilized eggs will be transferred. The embryo transfer is a simple procedure just like an IUI procedure. When the embryos are transferred on day 3, the embryo is said to be 8 cell stage.
Above video shows the procedure of transfer of Embryo under USG guidance.


When the embryos are transferred on day 5, it is at the blastocyst stage. This is the highest form of human life that can be sustained in the laboratory.
The number of embryos transferred will depend on the quality of the embryos and your previous discussion with the doctor.

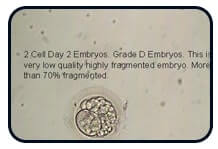



Depending on your age, anywhere from one to three embryos may be transferred. Recent studies have shown success with just one embryo transferred. The transfer will be done on a full bladder in the operation theatre. No fasting or special preparation is required for embryo transfer.
Embryo transfer does not require anaesthesia and is done on a daycare basis. When you come to our test tube baby centre in Mumbai in the morning, a routine vaginal scan is done to assess the endometrium. Then you will proceed to the recovery room, where the nurse will give you a progesterone injection. This will help in relaxing the uterus as well as maintaining good progesterone levels. You will lie down in the recovery room till your bladder is full. When the bladder is full, we take you to the operation theatre. There is soothing music which will help you to relax and be in a more positive frame of mind. At the time of transfer, the private parts will be cleaned with warm water and then the external catheter will be passed just beyond the internal OS.
The embryologist will then bring the internal catheter loaded with embryos. The selected embryos are transferred into the uterus by a specially designed catheter under ultrasound guidance, which helps to transfer the embryos in the correct place in the uterus i.e. 1-1.5 cm below the fundus which in turn increases pregnancy rates by up to 5-10%. After the transfer, you will lie down in the operation theatre for 10-15 minutes after which you will get up and go walking to the washroom and then lie down in the recovery room.
You may stay in our recovery room for a couple of hours (bring a book or your i-pad) and then head home. In the meantime, we will give you final instructions.
If there are “extra” good quality embryos left over, you may be able to freeze them. This is called “embryo cryopreservation.” They can be used later or destroyed or donated.
At our test tube baby centre in Mumbai on or after the day of your retrieval, and before the embryo transfer, progesterone preparations / other medications are given to enhance implantation (the process by which the embryo adheres to the uterus) and to support early pregnancy (Luteal Support). Progesterone preparations can be in the form of injections/oral tablets/vaginal tablets/vaginal gel. Generally, the dreaded painful injections (oil-based progesterone injections) are not given unless absolutely required. The vaginal tablets/gel and oral tablets have given equivalent or better results. These medications are continued for 14 days after the embryo transfer.
It has been noted that low plasma & high uterine levels following vaginal administration makes it unnecessary to monitor serum progesterone levels, thus providing substantial IVF cost savings in Mumbai.
Besides the progesterone, there really isn’t much going on for the next two weeks. In some ways, the two weeks after the transfer may be more difficult emotionally than the two weeks of treatment. During the previous steps, you will have visited your doctor perhaps every other day at Ankoor test tube baby centre in Mumbai . Now, after the transfer, there will be sudden lull inactivity. All you can do is wait for the two weeks and see if pregnancy takes place. It can help to keep busy with your life during this wait time and avoid sitting and thinking about whether or not treatment will be successful.
After fourteen days, a blood test – serum beta hCG is done to know the outcome of the cycle. No fasting is required for the test. We will get the report by afternoon and we will call you with the report.
If the test is positive, the blood test will be repeated every 5th day. This will help us to monitor the progress of your pregnancy. You will need to keep taking the progesterone supplementation for another several week. A transvaginal ultrasound is done when the beta hCG values reach a particular level. This will help us to monitor the pregnancy. At our test tube baby centre in Mumbai during every visit, your blood pressure and weight will be charted. Slowly the luteal phase support decreases and stops by 10-11 weeks. After this, the pregnancy continues as a routine pregnancy.
At our Test tube baby centre in Mumbai, we will also monitor whether or not the treatment led to multiple pregnancies. If it’s a high-order pregnancy (3 or more), the option of reducing the number of fetuses may be discussed. This is a procedure called a “multifetal pregnancy reduction.” This is sometimes done to increase the chances of having a healthy and successful pregnancy.
Male infertility is known to be associated (in some cases) with chromosomal and other genetic anomalies. There is known to be an increase in gross chromosomal abnormalities such as balanced translocation in men with very low sperm counts. Also, about 5% of men with very low sperm counts have small areas of missing DNA on their Y chromosome (Y micro-deletion). Techniques such as ICSI will, in some cases, may lead to transmission of genetic problems that might cause infertility in male offspring, or could possibly be associated with other (at this time unknown) medical problems in the child.
As of now, there have now been many thousands of babies born after IVF treatment with ICSI with follow-up after birth. Thus far, there has not been demonstrated to be any clear increased risk for birth defects as compared to IVF treatment with conventional insemination. Most studies thus far have shown that the risk of birth defects after ICSI is the same as for babies conceived through IVF treatment without ICSI, and for those conceived naturally. However, some studies have suggested that having IVF treatment with or without ICSI might increase the risk of birth defects.
Some studies have shown that around 4% of babies born via assisted reproductive technology such as in vitro fertilization (IVF treatment) may have major birth defects, such as heart and urogenital tract malformations. But these risks are not much different from what would be expected in the general population. The major birth defects seen in babies born via IVF treatment and/or ICSI included heart defects and malformations of the urogenital tract, such as hypospadias (an abnormality in the position of the opening of the urethra in boys).
It is not fully understood whether these birth defects or genetic diseases are caused by the infertility treatment itself or the underlying reason for infertility.
A total of around 8-10 visits are required to the clinic. Overnight hospitalization is NOT required.
The injections will not cause any weight gain.
But, you should refrain from high-impact exercise and choose workouts such as walking, swimming, yoga or cycling.
For Female Partners.
A transvaginal sonography is done to assess the ovarian reserve (how many follicles of 2-3 mm size on day 2/3 of cycle), endometrial thickness, subendometrial blood flow, to look for any other abnormalities that may be present like fibroid in the uterus, uterine septum uterine polyp adhesions.
Hormonal tests like serum FSH, LH, TSH, Prolactin and AMH.
Infectious disease tests like HBsAg, HCV, HIV
A hysteroscopy if required.
In most centers pre IVF hysteroscopy is a norm. But at Ankoor fertility clinic, we do not advise hysteroscopy as a routine to all IVF / ICSI patients. We do a thorough evaluation of the endometrium and its receptivity using Transvaginal ultrasonography (TVS) and Doppler studies. During these USGS we look for the endometrial thickness, echotexture, volume, and blood flow. If there is any abnormality in these studies, only then a hysteroscopy is advised.